Coping in Chaos
How to keep your cool when things get heated
25 MINUTE READ
Published August 2024
AUTHORS
Katie Sardone, PhD PMH-C
Head of Clinical, Licensed Psychologist & Perinatal Mental Health Specialist
Ann Dunnewold, PhD, PMH-C
Advisory Board, Licensed Psychologist
Rachel Oppenheimer, PysD
Contributing Editor, Licensed Psychologist
We all know that parenting is not for the faint of heart. With a little one at home, there are moments of well, sheer chaos! There are also glimmers of magic, most of which include those precious moments of connection with your child. This guide will help you identify what’s going on for you in those stressful moments and how to pump the breaks, cope and reconnect so you can experience more of the moments that make parenting meaningful.
Learning how to regulate your emotions
The foray into the first few months of parenthood can certainly be jarring. No matter how many parenting classes you take or books you read, nothing prepares you for dealing with intensely distressing crying, chronic sleep deprivation and the hopelessness and helplessness that can come with fumbling through the parenting learning curve. In these difficult moments it’s easy to lean in harder to “fixing” by meeting baby’s needs at the exclusion of your own. However, if you are only looking outward to solve the problem (“How can I stop this crying ASAP?!”) as opposed to staying grounded and tuned into your own needs (“Baby is doing what they need to do. How can I re-focus on myself; tag out, recuperate and tag back in when I’m ready to soothe baby?”) you may find yourself stuck in a frenzied and chaotic pattern.
Consistently ignoring or postponing your own needs may leave you stressed, overwhelmed, and eventually shut down¹. Ultimately, your baby needs YOU! Your baby doesn’t need perfection. It’s not about having the cutest onesie or the most perfectly manicured bassinet. To give your baby what they need requires both in-the-moment coping as well as taking care of yourself daily, so you can give them a whole, present and connected YOU! In this guide we’ll show you how to:
recognize when you are experiencing an acute stress response,
hit pause, and
downshift into a regulated and connected state so that you can pump the brakes and cope through the chaos.
Breaking it down further
All people experience stress. Stress is normal and necessary. It helps people motivate to do something different (like race across the room in the middle of the night to soothe a crying baby). Understanding the emotion of stress and what is going on in your mind and body can help parents have a greater sense of control and capacity to cope in those difficult moments². So let’s get into it, why on earth do we need to feel stress and what do we do with it?
The role of stress and emotion regulation in parenting
Our brains are designed to help protect us from threats we perceive out in the world. Threats could be things like seeing a wild animal in the woods, preparing for an annual review at work, or fear that you forgot to bring your baby’s formula to the playdate. The way in which we interpret this information from our environment, adapt, and respond can be boiled down to this basic biological process designed to help us, not to hurt us. Sometimes these automatic reactions, that often come without any warning, are right on target (like swerving your car out of the way when someone veers into your lane). Sometimes these reactions come when there isn’t an actual danger to you or your family (like when your child’s favorite sippy cup is nowhere in sight). What does this look like for parents?
We all have our own “triggers” for stress, but some of the common ones include:
Infant crying
Toddler tantrums
Sleep deprivation
Conflict with partners or family
Worry about baby’s immediate safety
Polyvagal theory and autonomous nervous system responses
Luckily for us - there is a LOT of research about how stress affects our bodies. Polyvagal theory³ is a theory that helps describe how our autonomous nervous system (ANS) innately responds to safe or dangerous/stressful situations. Before we dive into coping with stress, it’s first important to understand how stress manifests itself in our own bodies, and also how our reactions to stress impact our children. Both you AND your child have ANS reactions to stress.
There are three main ways the ANS responds to perceived safety or threats:
-
This is when our brains perceive that we are safe we can experience a sense of calm and connection with others. This is the ideal mental and physical state to be in, but we know that’s not always the case!
-
This is when our brain perceives an acute threat or stressor and is helping our body prepare to “fight” or “flee” from the problem. It’s a normal and helpful response as long as we use it when we need it and calm down when the stressor is over.
-
This state is brought on when our stress responses become chronic (overwhelming us) and our body is just shutting down.
What the ANS responses look like
SOCIAL ENGAGEMENT
Cool, calm and connected
-
Normal heart rate
Normal muscle tone
-
Calm
Relaxed
-
Relaxation
Engagement with others
Curiosity
Creativity
Hope and optimism
-
Can leave us vulnerable to threats, if we aren’t “activated” when we should be.
MOBILIZATION
Ready for fight or flight
-
Increased heart rate
Increased blood pressure
Increased hormone surge
Increased muscle tone
Changes in the gastrointestinal system
-
Anxiety
Fear
Worry
Panic
-
Provides energy
Drives motivation
Helps with physical activity
Playfulness
-
Can leave us vulnerable to threats, if we aren’t “activated” when we should be.-Stress
Anxiety
Fear
The “fight or flight” response
IMMOBILIZATION
Total overwhelm and shut down
-
Reduced heart rate
Reduced energy
Fatigue
Low muscle tone
-
Down
Lethargic
Depressed
Withdrawn
-
Meditative state
Blissful, calm
Dreamy
-
Hopelessness
Depression
Loneliness and disconnection
The “freeze” response
Understanding where you are on the ANS continuum
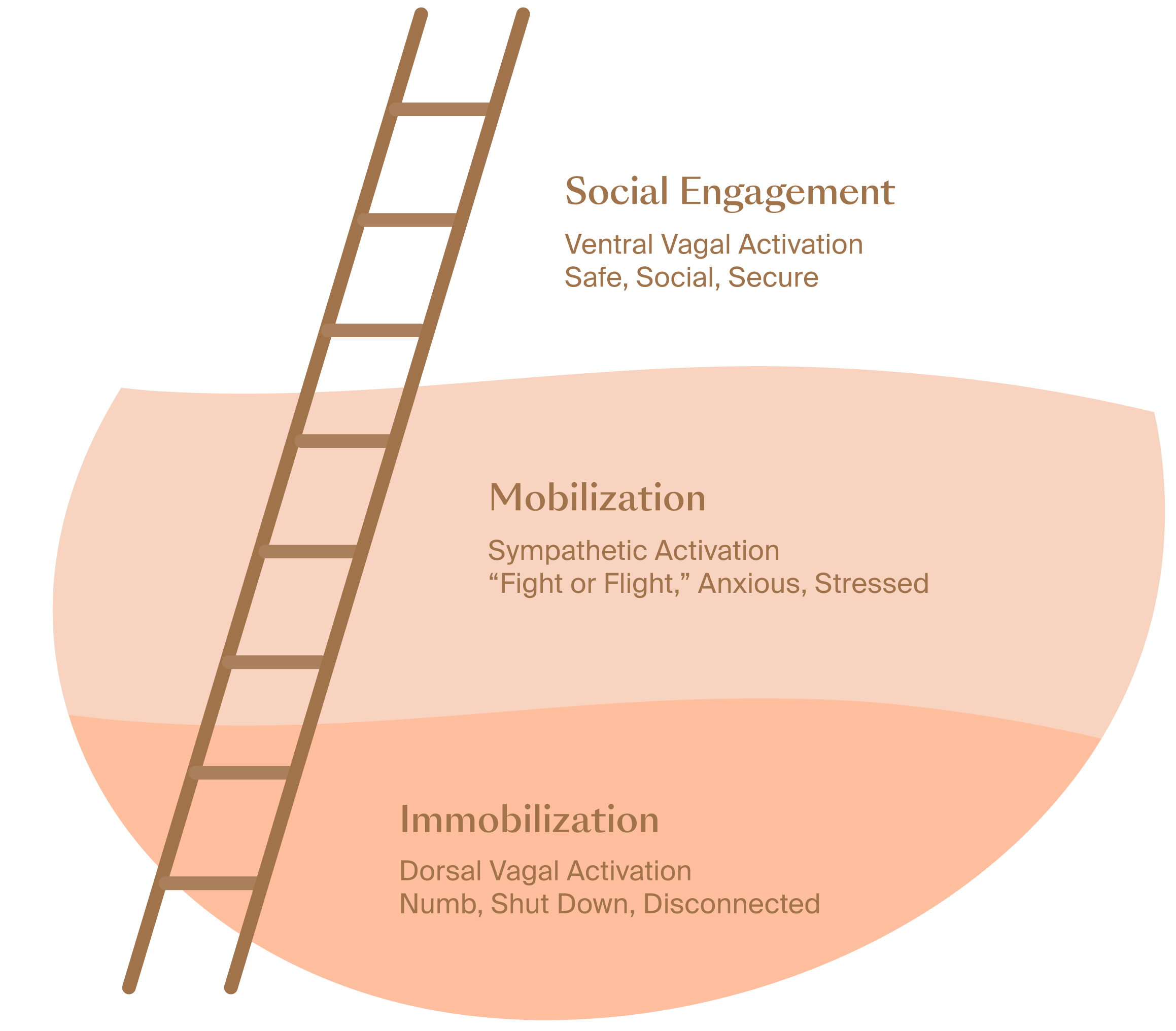
Being aware of where you fall on the continuum of these ANS responses is the first step toward coping and will help you decide how to best self-regulate and reconnect. If you view these ANS responses like steps of a ladder, you can imagine yourself going up and down the ladder of regulation in different situations. The top of the ladder represents safety and connection, what we hope to experience the most. The middle of the ladder, mobilization or “fight or flight,” is a short term experience that helps us in times of acute stress. Finally, the bottom of the ladder is immobilization or “shut down,” which is a result of chronic and intense stress which has not been resolved.
Take a minute to think about a situation when you’ve felt calm and notice what is happening in your mind (are you thinking optimistically, are you looking forward to something?) and your body (do you feel relaxed, is your heart rate normal and muscles relaxed)? What about when you’ve felt really stressed? What does that look like for you (a sense of panic, racing heart rate? Tense muscles? Butterflies in your stomach?). Finally, think about a time when you were past the point and felt total overwhelm. What happens to you personally in these moments (feeling like things will not get better, not wanting to be around others, wanting to stay home, and feeling down)? Beginning to identify what each ANS response state feels like for you is important so that you can recognize these states quickly and implement the strategies below to cope and reconnect.
Co-regulation and the ANS
Co-regulation is how one nervous system impacts another nervous system⁴. This happens all day long in all of our interactions with others. You can imagine how much your baby’s nervous system impacts yours (cut to screaming baby and panicked parent), but you may not be thinking about how your own nervous system is impacting your baby! The truth is we can almost “feel” and “sense” the emotions of others. Think of a time when you’ve been with a panicked friend or family member - did you notice that as they spoke quickly and out of breath about their problem that you started to feel your shoulders tense and notice you were holding your breath? This is an example of your friend’s ANS sending you signals that you should also feel worried because something is “wrong” - there is a perceived “threat.”
Co-regulation doesn’t only work in the negative direction. You can also use co-regulation strategies to help soothe another person. In the example above, with your friend, if you start talking in a calm, slower soothing voice, relax your face and body, and breathe slowly, this may in turn invite your friend’s ANS to downshift and regulate as well. As a parent, being aware of your own ANS responses and what you bring to the table is incredibly important (for more information on parental presence and connection check out our Essentials 0-6 month learning program). Young children require parental support for their own regulation (aka co-regulation) for the first few years of life. Parents have to model and eventually teach their children how to cope and regulate emotions. These skills learned early on can set a child up for success into childhood, the teenage years and even adulthood.
Let’s take a quick look at what co-regulation looks like for a parent and baby in the context of responding to ANS needs. If your baby could narrate the experience of their needs they might say “I’m cold, wet, alone, hungry. The fight or flight part of my system is activated. I need to fight (cry, scream, wail) to make sure my needs are met.” The way you meet your child’s needs in these moments sends a signal to their ANS in one way or another. If you respond in an anxious, panicked or angry manner (while in a mobilized or immobilized state) you’re sending the signal to your baby to stay in their mobilized, “fight or flight” state because something is “wrong.” On the flip side, if you’re able to:
recognize that you are in a mobilized state,
pause, and
take steps to regulate your own ANS response
then you can respond to your baby in a calm and connected manner - which as you now know means your baby will be invited to calm down as well. Just your calm and connected presence at that point is giving your baby a “tool” to calm themselves down.

What the research says
Learning to regulate your nervous system enhances mental well-being⁵.
Modeling self-regulation for your children allows them to learn to understand and regulate their own emotions effectively.⁶
The well-being of parents is a significant influence on the well-being of their children⁷,⁸.
Infants of mothers with high anxiety may be predisposed to “suboptimal nervous system development” which may lead to increased vulnerability for developmental problems such as motor problems and adverse emotional outcomes in childhood⁹.
Steps up the ladder to self-regulation
Good news! You have more control than you think over how you move up and down the ladder of regulation. Here are 3 steps to take when you notice yourself moving in the wrong direction:
Recognize that you are experiencing stress and identify where you are on the ladder of regulation
Use this chart to help you match your physical symptoms to the appropriate ANS state.
Hit pause and take a break!
Take a minutes long break to help yourself quickly assess the situation, realize that the threats you perceive are not imminent dangers, and move towards connection.
Choose a coping strategy from the list below to help your mind and body move back to the top of the ladder toward regulation and connection with others.
Grounding is a particularly helpful first coping strategy. You can remind yourself that in this moment you are safe, your baby is safe and you know this stressful experience will pass. (See below for more on grounding).
If you are feeling overwhelmed and agitated, make sure your baby is in a safe place first.
Place your baby safely in the crib, pack & play, or the arms of another adult.
Step away to allow yourself to regroup.
Remind yourself this break to manage yourself is best for you and your baby.
If you notice that you are having a difficult time coping, then tag someone else in.
Bring in your partner and tag out. If you are not with anyone else, consider calling a family member or friend. It is also helpful to have professional resources that are always available such as:
PSI Helpline
Call 1-800-944-4773 (4PPD) #1 En Español or #2 English
Text in English: 800-944-4773 Text en Español: 971-203-7773
988 Suicide and Crisis Hotline
Dial 988 - available 24/7 in Spanish and English

Coping strategies for calming and co-regulation
Since co-regulation is such an important part of helping us connect with our little one, and teaching our baby how to self-regulate in the world, many of the techniques that we offer can be incorporated within your everyday parenting routine.
It’s also important to keep in mind that if you find yourself at the “bottom of the ladder” (i.e. immobilized by stress) that it may take a little while to recognize the changes you need to make. Keep at it and consider asking your partner or a friend for help. Picking ONE thing from the list below that you commit to doing each time you feel stress is a meaningful step in the right direction. Coping is a skill that you'll get better at with time and practice. Once you’ve mastered one strategy below, you can add in new ones.
-
Why?
Slow, deep breaths tell our nervous system we are safe
Contrast with the rapid breathing when in “fight or flight.”
Focusing on the exhale can help slow down the breathing
How?
Blow bubbles
Imitate shuddering “horse lips”
Blow raspberries on babies tummy
Focus on the exhale, trying to make it longer than the inhale
-
Why?
Releases and redirects energy that’s stored to fight or flee.
Releases hormones such as endorphins, serotonin, dopamine
Stress release
How?
Pop the baby in a stroller, and go for a walk or a run (being outside in nature in good weather helps, too!)
Stretch
Bounce baby gently on your knee
Dance with the little one
Sway side to side, rocking yourself along with the baby
-
Why?
The vagus nerve run along the back of our throats
Vibrations along your throat are calming to the vagus nerve
Replaces the urge to yell or scream
How?
Hum
Sing
Gargle (especially with cool or cold water - see below on how cold can help too)
Buzz like a bee
Chant
-
Why?
A good laugh can activate the vagus nerve, calming you quickly.
Lifts mood and add levity
Also stimulates throat, and includes lots of exhaled deep breaths
How?
Watch a funny show
Read jokes or find memes about parenting
Even simulated laughter can be effective
Hearing laughter, like on a laugh track, can help¹⁰
-
Why?
Cold activates the vagus nerve.
Gives the body response something to focus on other than “fight or flight” by helping return your core body temperature to normal
Slows heart rate
How?
Splash water on your face
Take a cold shower, bath, or ice plunge while baby naps or is in the safe arms of another adult
Walk outside if it’s cold (and baby is well dressed)
Stick your head in the freezer
Run an ice cube along your neck, behind your ears, around your face
-
Why?
Increases awareness of body sensations
Helps focus the brain and body on the safety and reality of the here and now
Releases physical tension
How?
Go from head to toe, consciously tensing and relaxing muscles as you go.
Sing “Head, shoulders knees and toes” to your toddler as your mind focuses on these specific body parts to tense and relax
Imagine a ball of light healing and relaxing each part of the body progressing from the feet to the top of the head
Practice wiggling toes, clenching and unclenching fists, and flexing muscles along with your little one
-
Why?
The outer edge of the ear contains a branch of the vagus nerve, this is an area that can be touched subtly to help regulate and calm
Self-massage and self-compassion practices help calm the nervous system
How?
Pull on your earlobes
Softly trace your own outer ear, and then baby’s ear
Place your hand on your heart
Massage your own feet
Give yourself a hug
-
Why?
Ground yourself in the present! When your baby is crying even though you’ve met all their practical needs, remind yourself “My baby is safe and healthy. I am safe and healthy. We will connect and my baby will eventually calm down.”
Reduces heart rate and blood pressureSelf-massage and self-compassion practices help calm the nervous system
How?
Play “senses I spy,” focusing on something that can be seen, something that can be heard, something that can be felt, something that can be tasted, and something that can be smelled.
Play “A B Cs around the room,” see how far through the alphabet you can go by just labeling things surrounding you
Press your bare feet into the ground, feel the floor meet all parts of your feet
About the authors
Katie Sardone, PhD, PMH-C
Dr. Katie Sardone is a Licensed Psychologist and the founder of Behavioral Health Dallas, PLLC.
Rachel Oppenheimer, PhD, PMH-C
Dr. Rachel Oppenheimer is a licensed psychologist and licensed specialist in school psychology, licensed to practice in both Texas and Florida.
Ann Dunnewold, PhD
Ann has dedicated her career to guiding clients through the transition to parenthood. In addition to her role as a licensed psychologist, Ann has held numerous industry leadership positions.
Nutritionists
•
Adult mental health
•
Couples mental health
•
Infant & child mental health
•
Sleep coaching
•
Nutritionists • Adult mental health • Couples mental health • Infant & child mental health • Sleep coaching •
When to get
expert support
If you think you need expert support, this is a great reason to pop into office hours. Sometimes you might need more support, and that's okay! Here are times to reach out:
If you have thoughts of hurting yourself, the baby, or anyone else.
When it feels like the bad days outnumber the good days.
If you can’t stay on top of the bare basics of daily life - sleeping, eating, personal hygiene, other responsibilities.
If you feel like you know what you need to do, but you just don’t have the tools or resources to make it happen.
Have a question for your coach?
Schedule time during their weekly office hours! We know not all questions come up on a schedule, which is why your coach is also available outside of the sessions included in your Learning Program.
-
Le Vigouroux, S., Bernat, K., & Charbonnier, E. (2023). Risk factors and consequences of parental burnout: Role of early maladaptive schemas and emotion-focused coping. Trends in Psychology. https://doi.org/10.1007/s43076-023-00288-6
Jiménez, G. (2024, March 20). Pregnancy and childbirth reshape the brain in profound, sometimes lasting ways. Scientific American. https://www.scientificamerican.com/article/pregnancy-and-childbirth-reshape-the-brain-in-profound-sometimes-lasting
Porges, S. W. (2007). The polyvagal perspective. Biological psychology, 74(2), 116–143.
Porges, S. W. (2007). The polyvagal perspective. Biological Psychology, 74, 116–143.
Porges, S. W. & Dana, D. (2018) Clinical applications of the polyvagal theory: The emergence of polyvagal-informed therapies. W.W. Norton, Inc.
Edler, K., & Valentino, K. (2024) Parental self-regulation and engagement in emotion socialization: A systematic review. Psychological Bulletin, 150(2), 154-191.
Newland, Lisa. (2015). Family well-being, parenting, and child well-being: Pathways to healthy adjustment. Clinical Psychologist. 19, 3-14
Kingston, D., Tough, S. & Whitfield, H. Prenatal and Postpartum Maternal Psychological Distress and Infant Development: A Systematic Review. Child Psychiatry Hum Dev 43, 683–714 (2012).
Jelicic, L., Sovilj, M., Bogavac, I., Drobnjak, A., Gouni, O., Kazmierczak, M., & Subotic, M., (2021) The impact of maternal anxiety on early child development during the COVID-19 pandemic. Frontiers in Psychology, Psychopathology (12)
Fujiwara, Y., & Okamura, H. (2018) Hearing laughter improves the recovery process of the autonomic nervous system after a stress-loading task: a randomized controlled trial. Biopsychosocial Medicine, 12(22)